HIV is a dangerous and terminal infection. HIV is a complicated, encased pseudo-diploid RNA virus that attacks the immune system’s T-helper CD4+ cells. The p24 inner capsid protein, one of the nineteen encoded proteins, is one that can be made easily and is distinctive. Typically transmitted through sexual contact, HIV affects the immune system of the body.
DNA vaccines are the most common approach for creating an AIDS vaccine, and various volunteers are undergoing testing. Various AIDS vaccine development methodologies exist; however, they are less common: Recombinant vector and subunit vaccine development. Since many years ago, government and non-governmental organisations have generously funded the development of AIDS medicine through global giants like Mark and Vagen. As stated by Margaret Heckler, the then-US Secretary of Health and Human Services, an AIDS vaccine was expected to be available by the end of 1986. There has been no progress on an effective AIDS vaccine in the past 21 years. At the moment, AIDS vaccine trials are being supported by more than 3000 volunteers globally.
In the 1980s, the HIV virus was discovered for the first time in the US; since then, it has spread to other parts of the world. According to figures from 2020, there are over a million people in the US who may have HIV, and 14% of them are considered to be unaware of their illness. Though it is now mostly found worldwide, HIV primarily affects the African continent. According to the WHO’s estimate (HIV/AIDS), there were about 38 million new HIV cases worldwide in 2019 (HIV/AIDS). Therefore, it is imperative to gain more knowledge about the illness, including contributing causes, preventative measures, indicators, diagnoses, management techniques, and follow-up care.
People who contracted the virus in the early stages of the AIDS epidemic frequently died within a few years of becoming infected. People living with HIV and their allies’ outspoken campaigning and the steadfast efforts of supporters in the scientific community were among the factors that prompted the U.S. government to take action. They emphasised the necessity of developing effective medications, the necessity of enhancing access to effective medicines once they had been produced, and the significance of lessening the stigma associated with having HIV.
While there are several methods for preventing HIV infection, the creation of a secure and reliable HIV vaccine is still essential to permanently putting an end to the HIV pandemic. Researchers funded by NIAID are pursuing an HIV vaccine from two complementary angles: an empirical strategy that swiftly advances vaccine candidates into human testing and a theoretical strategy that develops vaccine candidates based on knowledge of the immune response to HIV infection.
When the massive RV144 trial’s findings revealed for the first time that an investigational vac cine regimen could impart a minimal level of protection against HIV infection, the effort to pr oduce a preventive HIV vaccine was given new life. NIAID and its international partners are still learning from and building on the results of this and other HIV vaccine trials today.
In order to quickly advance vaccine candidates into human clinical trials, an empirical approach to HIV vaccine developments based on observation is needed. In most trials for the AIDS vaccine, there was a chance that the volunteer would contract HIV. An eye-catching illustration is the Merck test from last autumn, which was a total failure and left many participants more susceptible to HIV infection. Merck has yet to offer any solid justifications for why the vaccine didn’t work.
Such events are provoking public outrage, and many scientists are urging a pause until fresh approaches to containing the AIDS virus’s ever-evolving nature are developed and implemented. According to Dr. Tony Fauci of the National Institute of Allergy and Infectious Diseases, since the STEP research was unsuccessful, we had to backtrack a little bit. There is now no realistic expectation that ongoing work on an AIDS vaccine will lead to any significant advancements. According to Mr. Desrosiers, one of the world’s leading authorities on the AIDS vaccine, “there is no rational basis for believing that any of the products in the pipeline have any reasonable hope of being effective.” Some clinical experts have suggested that developing a preventive HIV vaccine follow the iterative exploratory clinical trial method that has been successful in developing cancer treatment.
This paradigm uses several sequential trials to improve treatment plans, resulting in plans with increasing efficacy. HIV vaccine developers would employ iterative trials to guide the identification of immune responses that correspond with protection rather than merely fine- tuning vaccination schedules. While this plan is well-intentioned and creative, it ignores certain very fundamental differences that make it impossible to use it in the creation of an HIV vaccine. Cancer treatment methods may be evaluated on a small number of patients who are in grave danger of passing away quickly. So, relatively hazardous medications were tested by clinical scientists.
B-CELL IMMUNOGENS
After more than 10 years of diligent work, novel HIV vaccine candidates based on immunogens are currently being investigated in clinical settings. These immunogens are meant to activate B cells of the immune system to produce broadly neutralising antibodies (bnAbs) against the virus. This research’s beginnings can be traced back to the 2009 discovery of hitherto unrecognised, powerful bnAbs in sizable cohorts of HIV-positive people. The discovery of these antibodies ushered in a new phase in the creation of HIV vaccines. The target of all bnAbs, known as the HIV envelope or Env, has been identified by scientists by studying how these antibodies interact with the virus and neutralise it in laboratory studies.
To create vaccine immunogens, they have made use of this knowledge. Gaining insight into the structure of Env was another scientific advancement that fueled the invention of immunogens to generate bnAbs. For many years, the precise structure of this infamously brittle trimeric protein has eluded scientists, but recent developments have made it possible to stabilise Env and comprehend it in unprecedented detail. In particular, scientists have created and are testing synthetic vaccine immunogens that are intended to resemble the real structure of Env. Some of these ‘native-like’ trimers are being developed and clinically tested with help from IAVI. A Phase I clinical trial is being conducted at two sites in the United States and one in Kenya to assess one such candidate, BG505 SOSIP.664 gp140, adjuvanted.
HIV VACCINE TECHNOLOGIES
IAVI is engaged in significant research on vaccine technologies that enable the effective and efficient delivery of immunogens into the body. IAVI and its collaborators are looking into two technologies to reach this objective. Researchers at IAVI are largely concentrating on the vesicular stomatitis virus (VSV) as a replicating viral vector, which is one technology. They are developing a recombinant VSV vector that contains the HIV envelope gene and putting it through preclinical testing. Although the rVSV vector with the HIV gene insert is intended to be used as a prophylactic vaccination, this strategy may potentially be utilised therapeutically.
For Lassa fever, Marburg virus disease, Ebola Sudan virus disease, and COVID-19, IAVI is also working on rVSV-vectored vaccine candidates. Messenger RNA (mRNA) delivery is the second method IAVI is looking at for the purpose of delivering vaccine immunogens. mRNA directs the synthesis of proteins inside cells that your body needs to perform its many functions. It was first used in licenced vaccines for COVID- 19 and safely delivers instructions to cells to produce a SARS-CoV-2 protein that stimulates a protective immune response. IAVI and the biotechnology firm Moderna are examining the use of mRNA to transmit HIV antigens and trigger specific immune responses in IAVI G002 and IAVI G003.
CURRENT STATUS OF HIV VACCINE DEVELOPMENT
Researchers must first identify the correlate of protection from the prime-boost vaccination combination, or more specifically, how the prime-boost combination protected against HIV infection, in light of the favourable results from the RV144 study. Researchers have examined the antibodies produced by the prime-boost combination (which include a variety of antibody responses), the occurrence of T-cell responses, and whether the research participants’ unique genetics contributed to their reactions to the vaccine combination.
According to a 2012 study, the effectiveness of the vaccination was correlated with antibody responses to specific areas of viral envelope proteins, suggesting that T-cell responses did not likely contribute to immunity against infection. In an effort to use the insights gained from the largest HIV vaccine trial in history to enhance the design of subsequent trials, researchers are also examining the methodology and administrative strategies of RV144. The U.S. National Institutes of Allergy and Infectious Diseases and the U.S. government funded the trial for the two vaccines, which were first created by VaxGen and Sanofi Pasteur. The Army Medical Research and Materiel Command carried out the study’s execution through the efforts of numerous cooperating organisations, led by the Thai government. The trial involved extensive international cooperation between non-profit organisations, for-profit businesses, the Thai and American governments. In the opinion of vaccine developers, many lessons can be learned by looking beyond the results of RV144.
STRATEGIES FOR AN HIV VACCINE
Only a potent vaccine can stop the unchecked spread of HIV around the world and the lethal clinical effects of AIDS. Yet, some 20 years after the initial demonstration of HIV and its causal role in AIDS, this vaccine is still more of an aspiration than a reality. In this perspective, I discuss the particular challenges that the biology of HIV infection presents for the production of vaccines. I also provide a summary of recent developments in our understanding of the immunological control of HIV and its implications for vaccine development. I examine the justification for vaccinations with innovative designs and their trial results after examining the depressing history of unsuccessful conventional vaccine attempts.
HIV presents a particularly challenging target for the creation of vaccines. There is a genetically heterogeneous population of viruses among the HIV isolates that infect people and lead to AIDS. The HIV responsible for causing AIDS in much of West Africa is referred to as HIV-2; the HIV that causes AIDS throughout the rest of the world is referred to as HIV- 1. Because the genetic sequences of HIV-2 and HIV-1 are so different, their envelope glycoproteins frequently do not react with each other immunologically. Additionally, the HIV-1 virus family contains a variety of viral clades or subtypes that are epidemiologically concentrated in different geographical areas. These various clades of HIV-1 isolates differ from one another so dramatically in their genetic sequences and therefore in their antigenic characteristics that it has been suggested that different geographic regions of the world may actually require different vaccines. The parallel development of various region-specific HIV vaccines would clearly be both difficult and time-consuming.
Developing a vaccine against HIV is a particularly challenging goal. There is a wide variety of genetically different viruses among the HIV isolates that infect people and lead to AIDS. The HIV that causes AIDS across the rest of the globe is known as HIV-1, while the HIV that mostly affects West Africa is known as HIV-2. Since the genetic sequences of HIV-2 and HIV-1 are so different, their envelope glycoproteins frequently do not exhibit immunological cross-reactivity. The HIV-1 virus family also includes various viral clades or subtypes that are epidemiologically grouped in various geographical locations. A single HIV-infected person’s continued production of mutant virions due to the inefficient enzymatic machinery driving this virus’s replication also results in the constant generation of genetic diversity.
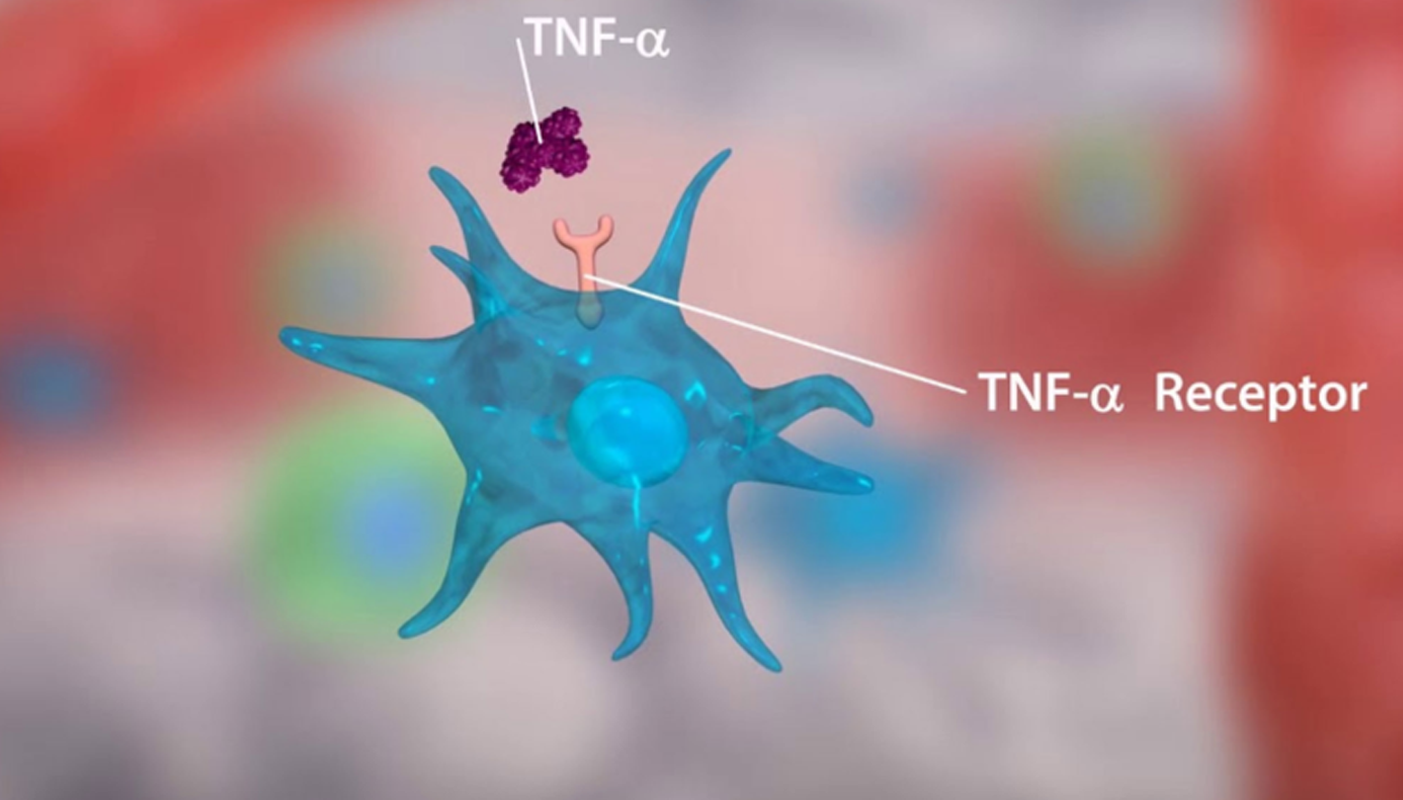
This process produces a population of virions that is so genetically diverse that an antibody that can neutralise one HIV isolate might not be able to neutralise another from the same person. HIV vaccine development is enormously complicated by the extraordinarily high level of genetic variability among HIV isolates. Other aspects of the biology of HIV infections also have substantial implications for AIDS vaccine development. HIV is transmitted both venereally and hematogenously. Therefore, there is reason to suppose that an effective HIV vaccine must elicit both mucosal immunity to contain sexually transmitted viruses and systemic immunity, to contain viruses transmitted directly into the bloodstream.
Furthermore, HIV is likely transmitted both as a cell-free and as a cell-associated virus. Therefore, more than a single type of immunity must be elicited by a vaccine if that vaccine is to be effective. Cell-free virions can be bound and neutralised by antibodies, while cell-associated viruses can be eliminated by cell-mediated immune responses. Finally, and most troubling for the prospects of developing an effective HIV vaccine, infection with this virus universally results in high levels of viral replication that persist in the face of seemingly robust anti-viral antibodies and cell-mediated immune responses.
HIV replication is never completely eradicated in humans, unlike the majority of other viral diseases. Moreover, the level and persistence of viral replication are inexorably tied to the pathogenicity of the virus, with high levels of persistent HIV replication being associated with rapid progression of clinical disease. The universal persistence of viral replication in spite of potent immune responses raises the spectre that no vaccine-elicited immune response may be capable of fully eliminating or containing HIV replication indefinitely.
The development of an AIDS vaccine is significantly impacted by additional features of the biology of HIV infections. HIV can spread hematogenously or through sexual contact. There is therefore reason to believe that a successful HIV vaccine must induce both mucosal immunity to prevent sexually transmitted viruses and systemic immunity, to prevent viruses that are directly transmitted into the bloodstream.
Furthermore, it’s probable that HIV spreads both cell-free and cell-associated forms of the virus. In order for a vaccine to be effective, it must stimulate the development of multiple types of immunity. Antibodies can bind to and neutralise cell-free virions, whereas cell-associated viruses can be killed by cell-mediated immune responses. Finally, and most concerning for the chances of creating an effective HIV vaccine, there is a universal HIV infection.
CONCLUSION
HIV is the most elusive virus, which presents a difficult challenge for the AIDS research community. There is currently no perfect vaccination that will completely protect against the virus due to its propensity to evolve into multiple resistant forms. Leading Merck researcher Dr. Susan Buchbinder claims that a fresh strategy is required if any noticeable outcomes are to be anticipated because “we have a huge epidemic on our hands.” Desrosiers also observes that the HIV virus has “the uncanny ability to replicate continuously, no matter what we throw at it. And we don’t even know what constitutes an effective immune response.” These opinions demand “going back” to the drawing board, re-evaluating, and conducting additional studies.
Close contact will have to be maintained between researchers and volunteers to avoid any complications resulting from AIDS vaccines. Clinical trials will have to continue, as they will form the basis for a new strategy in AIDS vaccine development.
Biotechnologist, VETA Genomics