Cystic fibrosis (CF) is a hereditary disease that affects thousands of people worldwide. It is a complex genetic disorder that primarily affects the lungs and digestive system, leading to significant health complications. It is caused by a defective gene that leads to the production of thick, sticky mucus, which obstructs the airways and impairs the functioning of various organs. Digestive complications arise due to the reduced release of digestive enzymes, causing malabsorption of nutrients and leading to malnutrition. CF also affects other organs, such as the pancreas, liver, and reproductive system.
The physical impact of CF on individuals can be debilitating, affecting their overall quality of life. CF poses significant challenges for those diagnosed with it and their families, requiring a multidisciplinary approach to manage the condition effectively. The history of CF dates back to ancient times, although it was not until the 18th centuary that the condition began to be recognized as a distinct entity. In 1938, Dr. Dorothy Andersen, a pathologisr, made a significant breakthrough by describing the characteristic changes in the pancreas of childern with CF. She coined the term “Cystic Fibrosis of the Pancreas” and laid the foundation for future research.
GENETIC BASIS AND PATHOPHYSIOLOGY OF CF
The genetic basis of cystic fibrosis lies in a mutation in a specific gene known as the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene. This gene provides instructions for the production of a protein called CFTR. The CFTR protein functions as a chloride channel on the cell surface, regulating the movement of chloride ions in and out of cells. It also plays a role in controlling the movement of other ions, such as sodium, across cell membranes. Chloride ions play a crucial role in maintaining the balance of salt and water in various tissues, including the lungs, pancreas, and digestive system.
CF is an autosomal recessive disorder, meaning that an individual must inherit two copies of the mutated CFTR gene, one from each parent, to develop the condition. People who carry only one copy of the mutated gene are considered carriers and typically do not exhibit any symptoms of CF. However, carriers can pass the mutated gene on to their children. The most common mutation associated with CF is known as the ΔF508 mutation, which accounts for approximately 70% of CF cases. This mutation involves the deletion of three nucleotides in the CFTR gene, resulting in the loss of a single amino acid (phenylalanine) in the CFTR protein. This structural change impairs the protein’s function, leading to the production of defective CFTR channels that do not transport chloride ions properly.
The absence or malfunctioning of CFTR channels disrupts the normal movement of salt and water across cell membranes. In the respiratory system, the impaired chloride secretion and increased sodium absorption cause dehydration of the airway surface liquid. This leads to reduced mucus clearance, accumulation of viscous mucus, and impaired mucociliary clearance. The thick mucus obstructs the airways, making CF individuals more susceptible to recurrent respiratory infections, inflammation, and progressive lung damage. In the digestive system, the malfunctioning CFTR protein affects the pancreas and its ability to secrete digestive enzymes. Without sufficient enzyme release, the digestion of fats, proteins, and carbohydrates is impaired, leading to malabsorption and nutrient deficiencies.
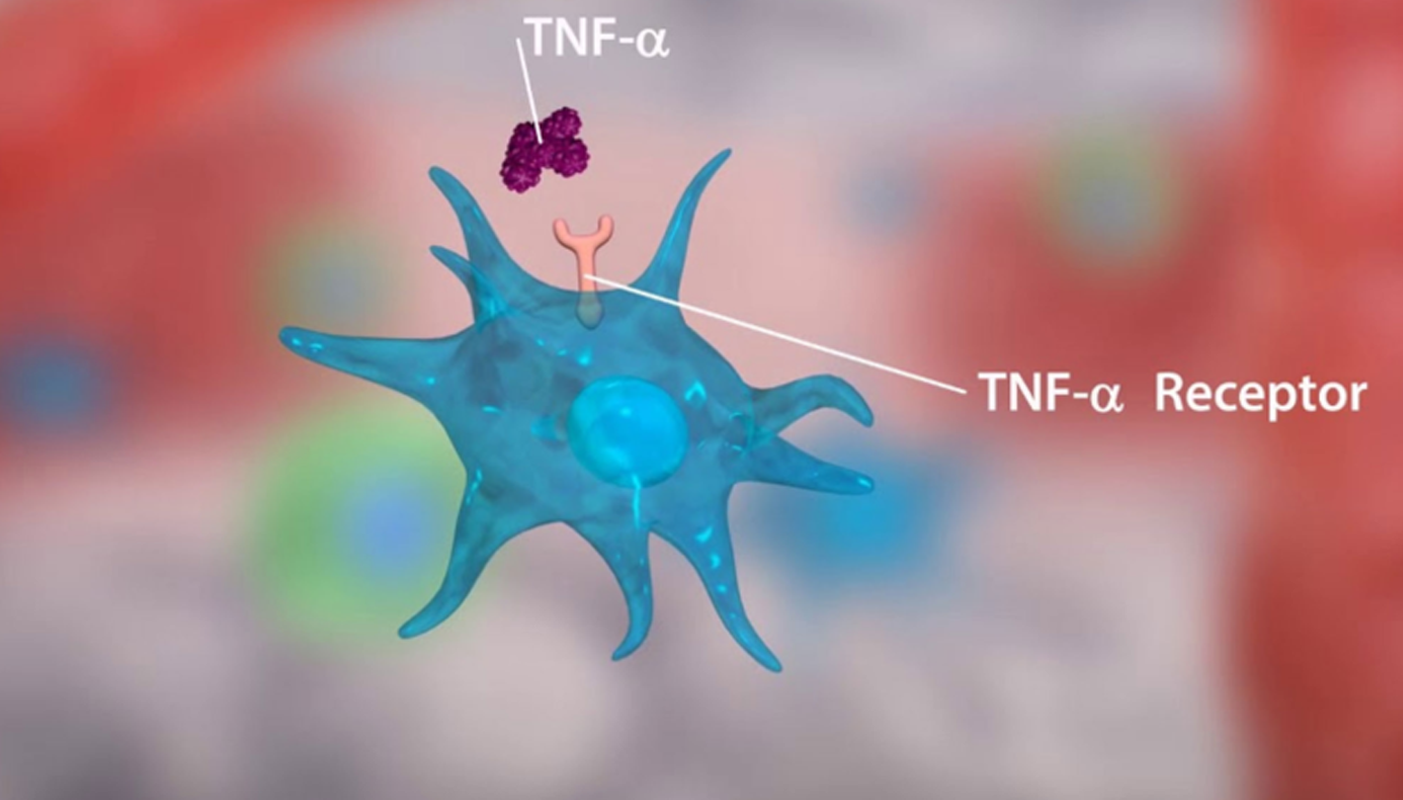
Additionally, the reduced bicarbonate secretion in the pancreatic ducts results in acidic conditions, which can contribute to pancreatic damage. The abnormal mucus characteristics in CF provide an ideal environment for bacterial colonization and recurrent infections. The thick mucus traps bacteria, allowing them to evade immune defenses and establish persistent infections. The impaired mucociliary clearance further compromises the ability to clear pathogens from the airways. Chronic inflammation is a hallmark of CF. The excessive release of pro-inflammatory cytokines, such as interleukin-8 (IL-8), attracts immune cells to the airways, resulting in a sustained inflammatory response. The continuous inflammation contributes to tissue damage, airway remodeling, and the progressive decline in lung function observed in CF. The sweat glands in CF individuals have increased chloride secretion, leading to elevated levels of chloride in sweat. This characteristic has been exploited in the diagnostic sweat chloride test for CF.
The reproductive system is also affected, with males often experiencing obstructive azoospermia due to the absence or obstruction of the vas deferens.CF-related liver disease can occur due to the accumulation of thick bile secretions in the small bile ducts. This can lead to biliary obstruction, inflammation, and the development of liver cirrhosis over time. While the ΔF508 mutation is the most prevalent, there are over 2,000 known mutations in the CFTR gene, each with varying effects on the protein’s function. The severity and progression of CF symptoms can vary widely among individuals depending on the specific mutation they carry. Understanding the genetic basis of cystic fibrosis has been instrumental in developing diagnostic tests, genetic counseling, and targeted treatments. Newer therapies, such as CFTR modulators, aim to correct the underlying genetic defect and improve the function of CFTR channels, offering significant hope for individuals with CF and their families.
CLINICAL MANIFESTATIONS AND DIAGNOSIS OF CYSTIC FIBROSIS
The clinical manifestations of CF can vary widely among individuals, but certain characteristic symptoms and complications are commonly associated with the condition. Early diagnosis is crucial for initiating appropriate treatment and management strategies. Newborn screening programs and diagnostic tests such as the sweat chloride test and genetic testing have greatly improved the accuracy and efficiency of CF diagnosis. Continued research and advancements in diagnostic tools and therapies offer hope for early intervention and improved outcomes for individuals with cystic fibrosis.
1. Respiratory Manifestations: The respiratory system is primarily affected in CF due to the production of thick, sticky mucus that clogs the airways and impairs lung function. The respiratory manifestations of CF include:
a) Chronic cough: Persistent cough is often one of the earliest symptoms of CF. It may be productive, with the production of thick sputum.
b) Recurrent respiratory infections: Individuals with CF are prone to recurrent lung infections, including bronchitis and pneumonia. These infections can lead to chronic inflammation and lung damage over time.
c) Shortness of breath: Obstruction of the airways and compromised lung function can result in shortness of breath, especially during physical exertion.
d) Wheezing: Constriction and narrowing of the airways can cause wheezing, a high-pitched sound during breathing.
e) Clubbing: Clubbing is the enlargement and rounding of the fingertips and toes, often seen in advanced stages of CF. It is a result of chronic hypoxia and poor oxygenation.
2. Digestive Manifestations: CF affects the digestive system, leading to various gastrointestinal manifestations. These include:
a) Malabsorption: The thick mucus in the pancreas obstructs the release of digestive enzymes, impairing the absorption of nutrients. This can result in malnutrition, poor weight gain, and vitamin deficiencies.
b) Steatorrhea: Malabsorption of fats leads to the passage of greasy, foul-smelling stools.
c) Meconium ileus: Newborns with CF may present with a blockage in the small intestine known as meconium ileus. This requires immediate medical attention.
d) Pancreatitis: Inflammation of the pancreas can occur, leading to abdominal pain and impaired pancreatic function.
3. Other Manifestations: CF can also affect other systems in the body, leading to additional manifestations such as:
a) Salt loss: The dysfunction of sweat glands in individuals with CF results in excessive salt loss through sweat. This can lead to electrolyte imbalances and dehydration.
b) Infertility: Men with CF often have a reduced fertility rate due to the absence or blockage of the vas deferens. Women may experience fertility issues due to the abnormal cervical mucus.
c) Diabetes: CF-related diabetes (CFRD) is a specific type of diabetes that can develop in individuals with CF due to pancreatic damage and impaired insulin production.
4. Diagnostic Process: Diagnosing cystic fibrosis involves a combination of clinical evaluation, family history assessment, and laboratory tests. The diagnostic process includes the following steps:
a) Newborn screening: Many countries have implemented newborn screening programs for CF. A blood test is conducted to detect elevated levels of a protein called immunoreactive trypsinogen (IRT), which is indicative of CF. Positive screening results are followed up with additional diagnostic tests.
b) Sweat chloride test: The sweat chloride test is considered the gold standard for CF diagnosis. It measures the chloride concentration in sweat, as individuals with CF have abnormally high levels of chloride due to dysfunctional CFTR protein. A sweat sample is collected and analyzed to determine the chloride level.
c) Genetic testing: Genetic testing is performed to identify specific CFTR gene mutations. DNA analysis can detect common CFTR mutations, including the ΔF508 mutation, as well as rare mutations associated with CF.
d) Clinical evaluation: The clinical evaluation involves assessing the individual’s symptoms, medical history, and physical examination. Pulmonary function tests, chest X-rays, and other imaging studies may be conducted to evaluate lung function and identify any structural abnormalities.
e) Other tests: Additional tests may be performed to assess pancreatic function, liver function, and nutritional status. These may include blood tests to measure pancreatic enzymes, liver function tests, and assessments of nutrient levels.
PREVALENCE AND INCIDENCE
CF is considered one of the most common autosomal recessive disorders, affecting diverse ethnic groups. The prevalence of CF varies geographically, with higher rates observed in populations of European descent. In North America and Europe, the estimated prevalence ranges from 1 in 2,500 to 1 in 3,500 live births. However, CF is increasingly recognized in populations beyond these regions, including Asia, Africa, and Latin America. The incidence of CF also varies across populations, with higher rates reported in certain regions. Factors such as consanguineous marriages and founder effects contribute to higher incidence rates in specific ethnic groups.
1. Genetic variations and mutation frequencies
CF is caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. More than 2,000 CFTR gene mutations have been identified, with varying frequencies among different populations. The most common CFTR mutation worldwide is the ΔF508 mutation, which is found in approximately 70% of CF patients. However, the distribution of other CFTR mutations varies across populations, highlighting the importance of genetic diversity in CF epidemiology.
2. Demographic factors and socioeconomic status
Certain demographic factors and socioeconomic status can influence CF epidemiology. Gender plays a role, as CF affects both males and females, with similar prevalence rates. However, differences in clinical manifestations and disease progression have been observed between genders. Socioeconomic factors, such as access to healthcare, genetic screening, and diagnostic services, can impact CF diagnosis and management. Disparities in CF outcomes may be influenced by socioeconomic status, highlighting the need for targeted interventions to ensure equitable access to care.
3. Regional differences and international variations
CF epidemiology exhibits regional differences and international variations. In regions with higher CF prevalence, such as Europe and North America, there are well-established CF registries that track patient data and facilitate research. These registries provide valuable insights into disease patterns, genotype-phenotype correlations, and treatment outcomes. In contrast, CF is relatively under-recognized in many low- and middle-income countries, leading to challenges in accurate prevalence estimation and resource allocation. Limited access to genetic testing, diagnostic facilities, and specialized CF care contributes to underdiagnosis and delayed management in these regions.
4. Changing epidemiology and global health initiatives
The epidemiology of CF is evolving, influenced by factors such as improved diagnostics, newborn screening programs, and advancements in CF care. Early diagnosis through newborn screening has become standard practice in many countries, enabling early intervention and improved outcomes. Global health initiatives, such as the Cystic Fibrosis Foundation’s Global Initiative and the World Health Organization’s efforts to improve CF care, aim to enhance access to diagnosis, treatment, and care for individuals with CF worldwide. Collaborative research efforts and international partnerships are vital in addressing the global burden of CF and ensuring equitable healthcare for all. Understanding these epidemiological aspects is crucial for healthcare planning, resource allocation, and the development of targeted interventions. By fostering international collaborations and promoting equitable access to care, we can strive towards improved outcomes and a better quality of life for individuals living with cystic fibrosis across the globe.
RESEARCH AND FUTURE PERSPECTIVES OF CYSTIC FIBROSIS
Research in cystic fibrosis has made significant strides in recent years, leading to improved understanding, diagnosis, and treatment options. CFTR modulator therapies have revolutionized the management of CF, while emerging therapeutic approaches such as gene editing, RNA-based therapies, and proteostasis modulators offer new avenues for treating individuals with rare CFTR mutations. Additionally, research on lung regeneration, microbiome, gene therapy, and holistic care models aims to enhance the quality of life for individuals with CF.
1. Genomic Research and Precision Medicine: Advancements in genomics and the availability of high-throughput sequencing technologies have greatly contributed to our understanding of the genetic basis of cystic fibrosis. Large-scale studies, such as the Cystic Fibrosis Foundation’s Patient Registry and the International Cystic Fibrosis Gene Modifier Consortium, have facilitated the identification of rare CFTR mutations, genetic modifiers, and their impact on disease severity. This knowledge has paved the way for the development of personalized or precision medicine approaches, where treatments can be tailored based on an individual’s specific genetic profile.
2. CFTR Modulator Therapies: One of the most significant breakthroughs in CF research has been the development of CFTR modulator therapies. These medications target the defective CFTR protein directly and aim to restore its function. Currently, three CFTR modulator drugs are approved by regulatory authorities: Ivacaftor, Lumacaftor/Ivacaftor combination, and Tezacaftor/Ivacaftor combination. These therapies have shown remarkable clinical benefits, improving lung function, reducing exacerbations, and enhancing overall quality of life for individuals with specific CFTR mutations.
3. Emerging Therapeutic Approaches: While CFTR modulator therapies have been a game-changer for many CF patients, they are effective only for specific CFTR mutations. Ongoing research focuses on developing novel therapeutic approaches to address the needs of individuals with rare or complex CFTR mutations. Some of these emerging approaches include:
a) Gene Editing: Gene editing technologies, such as CRISPR-Cas9, hold promise for directly correcting CFTR gene mutations. Although still in the experimental stage, gene editing techniques offer the potential to provide a more definitive and long-lasting treatment for CF.
b) RNA-Based Therapies: RNA-based therapies, such as RNA interference (RNAi) and antisense oligonucleotides (ASOs), are being explored as potential strategies to modulate CFTR expression and function. These therapies aim to correct or bypass the defective CFTR gene, providing a more universal treatment approach.
c) Proteostasis Modulators: Proteostasis refers to the cellular processes involved in protein folding, degradation, and quality control. Disruptions in proteostasis have been implicated in CF pathogenesis. Research is underway to develop small molecules known as proteostasis modulators, which can correct abnormalities in protein folding and enhance CFTR function.
4. Lung Regeneration and Repair: Another exciting area of research in CF focuses on regenerative medicine and lung repair. Strategies to promote lung regeneration include stem cell-based therapies, tissue engineering, and the use of growth factors and cytokines to stimulate tissue repair and regeneration. These approaches aim to restore damaged lung tissue and improve lung function in individuals with advanced CF-related lung disease.
5. Microbiome and CF: The study of the lung microbiome, which refers to the collection of microorganisms in the lungs, has gained significant attention in recent years. Researchers are investigating the intricate relationship between the lung microbiome and CF, including how dysbiosis (imbalance) in microbial communities contributes to lung inflammation and infection. Understanding the role of the microbiome may open avenues for developing novel therapeutics that target the microbiota to promote a healthier lung environment.
6. Gene Therapy: Gene therapy approaches aim to deliver functional copies of the CFTR gene to affected cells, thereby restoring normal CFTR protein expression and function. While progress in gene therapy has been slow due to challenges such as efficient delivery of the gene to target cells and long-term expression of the gene, recent advancements, such as the use of viral vectors and lipid nanoparticles, have shown promise in preclinical and early-stage clinical trials.
7. Improving Quality of Life: Research efforts in CF extend beyond therapeutic approaches to focus on improving the overall quality of life for individuals with CF. This includes psychological support, mental health interventions, nutritional interventions, and comprehensive care models that address the holistic needs of CF patients and their families. The future holds great promise for further advancements in CF research, offering hope for improved outcomes and ultimately finding a cure for this complex genetic disorder.
CONCLUSION
Cystic fibrosis remains a challenging disease, but significant progress has been made in understanding its underlying mechanisms and developing novel therapies. Advances in genetics, personalized medicine, and gene-editing technologies offer hope for improved treatments and better outcomes for individuals with CF. While there is still much to discover, the tireless efforts of researchers and the resilience of CF patients and their families continue to push the boundaries of medical science, giving rise to a future where CF may no longer be a life-limiting condition. Through multidisciplinary care, early diagnosis, and ongoing research, we are inching closer to a world where individuals with cystic fibrosis can lead longer, healthier lives with improved quality of life. The collective efforts of healthcare professionals, researchers, patients, and their families are crucial in raising awareness, advocating for better resources, and supporting advancements in CF treatment and care. Together, we can strive for a future where CF is better understood, effectively managed, and ultimately cured.
Biotechnologist, VETA Genomics